A new staffing measurement recommended in a major review of how the NHS can become more efficient fails to recognise the complexity of care provided by nurses and could lead to unsafe staffing levels, workforce experts have warned.
They cautioned that the introduction of the metric – which measures how many hours of care are provided collectively by registered nurses and healthcare support workers per patient in a 24 hour period – could begin a “race to the bottom” on what were deemed adequate staffing levels.
“You could have a fabulously staffed ward in the daytime and terribly staffed ward at night time and this measure won’t reveal that”
Jane Ball
The metric, called the care hours per patient day (CHPPD), should become the “principal measure of nursing and care support deployment” – from as early as April this year, according to Lord Carter’s efficiency review final report published yesterday.
The review proposed that hospitals be benchmarked against an average CHPPD range, which would be defined by the new regulator NHS Improvement, in collaboration with the chief nursing officer for England, the Royal College of Nursing and other organisations.
In his review, Lord Carter worked with 32 hospitals over 18 months to look at their challenges and how to improve productivity.
Analysis of data from over 1,000 wards found a wide variation in the care hours provided per patient day – ranging from 6.33 to 15.48 hours, with an average of 9.1 hours.
- Tackling delayed discharge key to NHS savings, says Carter
- Carter review recommends new measure of nurse productivity
- Carter review to back new measure of nurse productivity
The report suggested that, in the future, wards with similar speciality, length of stay, layout and patient acuity and dependency could compare their CHPPD figures and “consider if variation is unwarranted, to assist productive ward initiatives”.
The new measurement has been developed from staffing metrics already used internationally in Australia, New Zealand, and the US, which see efficiency reviewed within a CHPPD range by checking variation at ward level on a daily basis.
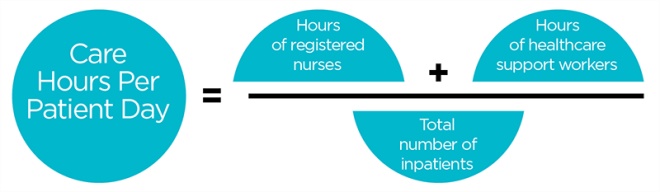
The metric for the NHS will be calculated by adding the hours of registered nurses to the hours of healthcare support workers and dividing the total by every 24 hours of inpatient admissions.
“This doesn’t take into account any care that is left undone. It gives us an average of hours of care”
Alison Leary
The report noted: “Conventional units of measurement – such as reporting staff complements using whole-time equivalents, skill-mix or patient to staff ratios at a point in time – may not reflect varying staff allocation across the day.”
But concerns have been raised about a number of issues with the new metric, including that it does not recognise the different types of care provided by registered nurses and healthcare support workers.
Professor Alison Leary, chair of healthcare and workforce modelling at London’s South Bank University, described the new metric, based on averages, as “a blunt instrument for a complex situation” and warned it could be a “race to the bottom”.

Alison Leary
Alison Leary
“It’s a complex relationship between staffing and safety… this [metric] isn’t a reflection of that complexity, so it’s hard to see how it would be helpful in ensuring safe staffing,” she told Nursing Times.
“This doesn’t take into account any care that is left undone for one thing. It gives us an average of hours of care,” she added.
Jane Ball, a nursing workforce expert from Southampton University and former deputy director of the National Nursing Research Unit at King’s College London, also raised concerns about making staffing decisions on the basis of the metric.
She said it was a “fatal flaw” to measure hours of care by registered nurses and healthcare support workers together.

Jane Ball
Jane Ball
“To arrive at a metric that is a merger of registered nurse staffing and healthcare support worker staffing is a fatal flaw in terms of ensuring safety,” she said.
She also said measuring hours of care per day in this way – even if it just focussed on registered nurses – would just provide an average over 24 hours and, therefore, used in isolation could hide shifts with unsafe levels of staff.
“The problem with that is, you could have a fabulously staffed ward in the daytime and terribly staffed ward at night time and this measure won’t reveal that,” she said.
Ms Ball said the use of nurse-to-patient safe staffing ratios alongside the metric would help to avoid this, but warned there was a risk trusts would pay too much attention to the new measurement requirement.
In response, a Department of Health spokeswoman told Nursing Times it expected the CHPPD metric to be one factor trusts took into account when making decisions on safe staffing.
Nursing workforce experts question new staffing metric
Lord Carter’s review, which made 15 recommendations in total in a bid to help NHS hospitals save £5bn a year by 2021, also found a “vast” variation in the use of “specialling” across the sample of trusts being analysed.
It pointed to one trust that saved £1m by adopting a “rigorous” policy for managing this type of one -to-one care, which it suggested should in the future be referred to as “enhanced care”.
A good practice guide and national programme for tackling variation in specialling across the service should be developed, with acute trusts implementing changes by October, it added.
Meanwhile, a “significant proportion” of the £5bn saving will not be unlocked unless delays in transfer are managed more effectively, said Lord Carter.
His report found that while official NHS England statistics showed an average of 5,500 patients per day were delayed, information provided by acute trusts revealed a worse problem with up to 8,500 per day unable to leave.
It estimated the cost of these delays to be around £900m to NHS providers.

Carter review to back new measure of nurse productivity
Lord Carter
To tackle this, the report recommended the Department of Health, NHS England and NHS Improvement work with local government on a strategy to help trusts ensure patients can be moved out of hospital as soon as they are ready.
In addition, the report said motivation and morale among the NHS workforce needed to be addressed in order to improve performance and productivity.
It noted sickness and absence rates varied from 2.7% to 5.8% across the trusts in its sample and highlighted the “alarming” high rates of alleged bullying and harassment reflected in the annual NHS staff survey.
NHS workforce data also suggested poor retention of staff in the service, said the report, with 121,000 new staff joining in the year to August 2015, but the number of employed staff only rising by 18,000 in the same time.
The report’s recommendations included more regular staff reviews, improved management practices to understand attrition rates, and a reduction in bullying and harassment through a campaign led personally by each trust chief executive.
 Nursing Times Resources for the nursing profession
Nursing Times Resources for the nursing profession


Well at least they are admitting what I have been saying for years, it’s all about the money and nothing to do with improving patient care. Enough savings to employ a couple more pen-pushers to oversee it.
Same old same old.
Jane Ball quoted:
‘She also said measuring hours of care per day in this way – even if it just focussed on registered nurses – would just provide an average over 24 hours and, therefore, used in isolation could hide shifts with unsafe levels of staff.’
I’ve pointed out in an earlier piece about this new measure, that it does NOT so far as I can see address:
The report noted: “Conventional units of measurement – such as reporting staff complements using whole-time equivalents, skill-mix or patient to staff ratios at a point in time – may not reflect varying staff allocation across the day.”
So I agree with Jane.
I think I don’t agree with some of the other criticisms, because I thought I’d seen something saying that RCN and HCA numbers were to be counted separately ?
Probably, any measure able to be implemented, will ‘theoretically fall somewhat short’ – the most important thing is to make sure the measure seems helpful, and ‘cannot be gamed’.
You don’t have to be an expert to work this one out = the only difference is who is better regarded in their critique. But lets be honest what a load of bull.
Care delivered by a Registered Nurse can include informal assessments as part of the process of washing, bathing, turning, mobilising etc. Whilst healthcare support workers may provide valuable input based on experience they rarely have similar levels of training and preparation as Registered staff.
This equation is of care, not PROFESSIONAL care which is very different. It is quite concerning how rapidly the analysis that came in the Francis Report amongst others appears to be pushed to one side.
The difference in recovery rates and economics of better trained/graded has been long established by the York Centre for Health Economics but it appears that as sufficient graduates are not being attracted to the profession we are on a downward spiral again towards a workforce of yesteryear.
Why don’t they measure it on nurse burnout and retention rates? DOH
The nursing professions spokespeople ( you know them all) have not focussed on articulating the value and complexity of nursing – choosing to focus on what parts of the doctors role they can take to make more and more advanced specialisms. The battle is lost folks and nursing lost the plot in the mid 1980s when Project 2000 began. The real complexity and value of nursing was in remaining generalists not specialising before qualification. Articulating our case was hence split amongst 5 branches and we lost respect.
How on earth will they assess the time it takes a registered theatre nurse to care for perioperative patients in mind of how complex that role is along with what is involved in that role?
As I understand it the Australian system is more complex than suggested. Firstly the Australian NHPPD is calculated using only registered nursing hours of those providing direct care as their main function. Other staff, even if they are registered nurses such as Ward Managers are not included. Furthermore patient hours combine not just hours present but also patients’ acuity and dependency needs. Seven ward types (A to G) are identified each of which has a different NHPPD. For high complexity wards (A) this is 7.50 hours per patient for Ambulatory Units (G) it is 3.00. These ward types are based on a previous assessment of patient acuity and dependency and nursing workload. All patient hours are included even if a patient spends less than 24 hours on the ward as are ward factors such as the number of admissions and discharges. This combination provides a much more comprehensive and multi-faceted assessment.
NHPPD has already been used in at least on eacute Trust to my knowledge. So rather than spending time and resources on a ‘new’ metric why not ask all Trusts to apply the Australian system? This would not only allow for comparisons between those Trusts but also with similar acute wards in Australia.
I don’t understand any of it to be quite frank…. ….how much time per hour can a nurse spend with a patient ?
Been there, done that! Doesn’t works! Consumes a lot of nurse hours /day filling out the forms and doing complicated calculations which could have been spent with patients carrying out essential care. Instead of this the completed paperwork becomes the central focus and then only to discover there often aren’t enough staff to fill the hours needed as a result of the findings. Staff have to be taken from other areas leaving a shortage there. Also the workload is difficult to forecast with any accuracy as it is constantly changing depending on the state of patients and their clinical and other needs at any one particular time. The programme also cost a lot to purchase and to implement.
Who are you trying to impress now MICHAEL STONE.
To 8 FEBRUARY, 2016 9:37 PM
Bingo you’ve hit the nail on the head – they will not measure this as it will fly in the face of government ideology, which is tough regimes built on less staff more process without intellect, such as promoted by Carter. What you have mentioned in modern day terms is called and I quote methods resulting in ‘ LEAN CARE DELETISM’ “, look to American hospital review sites to see what ground staff are saying to get the hint on staffing. LEAN CARE DELETISM is the result of staff stress and high turnover based on inappropriate use of fixed variable tools to care tasks based on economic resolve resulting in false measures of safe practice, often supported by behavioural solutions to surpress external factors arising. Perversely it results in less time with patients – there are hint to what is happening in the UK at the moment such as staffing issues reported by the CQC. Also question why is there such preoccupation with processes in hospitals where so much has gone wrong with staffing – the answer I suspect is not that people are questioning faulty methodology their coming up with we must do the wrong methodology better. And to make matters worse the government seem to be advocating this response. Carter’s and government approach and the Union Bill is a danger to proven health and safety legislation. When we have a weak HSE, weak unions and an altering of conception to what HaS is by government then both patients and staff suffer. We are all suffering at the hands of poor government ideology and those who blindly follow. And guess what you don’t have to be on the left side or even political to recognise these things.
We support human being who are multi faceted dynamic beings. they need time not only to nurse but to listen to a vast range of fears and emotions. Nursing is complex ,challenging as well as rewarding. But not necessarily financially
Excellent comment from Anonymous 17.2.26 5.45 pm.
Financial isn’t the greatest or even the best reward, but nurses have to live and have a need to be recognised, valued and rewarded for all of their hard and essential work like any other.
Care hours per patient per day = a general input of two very diferent types of care, also too simple a tool: it does not recognise the changing dynamics of lets say, hour by hour changes in patients’ condition due to
detoriating patients or change of patients on the ward.
Untill a very intelligent tool can be have I would advise to stay clear of any tool that is too basic for a work environment that has so many variables.