In women, pelvic floor weakness can lead to incontinence or prolapse. This article – the first in a two-part series – describes the female pelvic floor anatomy and pathophysiology
Abstract
In women, the pelvic floor muscles are put at risk of damage and dysfunction by a series of factors such as high-impact exercise, obesity, pregnancy and childbirth, chronic constipation and the menopause. A weakened pelvic floor can have two major negative consequences: incontinence (urinary and/or faecal) and pelvic organ prolapse. This two-part series discusses what nurses need to know about the female pelvic floor and how to help women look after it. Part 1 describes the anatomy of the female pelvic floor, along with the causes of, and risk factors for, pelvic floor weakness and the symptoms with which women may present. Part 2 discusses how to assess pelvic floor health and teach women rehabilitation exercises.
Citation: Yates A (2019) Female pelvic floor 1: anatomy and pathophysiology. Nursing Times [online]; 115: 5, 18-21.
Author: Ann Yates is director of continence services, Cardiff and Vale University Health Board.
- This article has been double-blind peer reviewed
- Scroll down to read the article or download a print-friendly PDF here (if the PDF fails to fully download please try again using a different browser)
- Read part 2 of this series here
Introduction
The pelvic floor is a complex group of muscles that exists in both males and females. Pelvic floor muscles have a multitude of functions, one of the most important of which is to help maintain urinary and faecal continence.
Continence issues can affect the bladder, bowel or both. Incontinence is prevalent in the UK, with an estimated 14 million adults experiencing urinary incontinence (NHS England, 2018; NHS England, 2015) and over 6.5 million having bowel control problems (Yates, 2017; NHS England, 2015). In women, the most prevalent types of continence problems are:
- Stress urinary incontinence, which affects 10-39% of women;
- Mixed urinary incontinence, which affects 7.5-25% of women;
- Urge incontinence, which affects 1-7% of women (Abrams et al, 2017).
Approximately 10% of all adult women experience urinary leakage at least once weekly and 25-45% experience occasional leakage (Abrams et al, 2017).
There is a lack of knowledge among women about pelvic floor dysfunction (De Andrade et al, 2018), despite the fact that pelvic floor rehabilitation can improve, or even cure, symptoms of incontinence (Dumoulin et al, 2018). This two-part series discusses what nurses need to know about the female pelvic floor: part 1 covers the anatomy and functions of the female pelvic floor, why it can become weak or dysfunctional, and how this manifests symptomatically; part 2 covers pelvic floor assessment and rehabilitation, with practical guidance on how to examine patients and how to teach them pelvic floor exercises.
Pelvic floor anatomy
The female pelvic floor is made of muscles and connective tissue that form a ‘sling’ or ‘hammock’ across the base of the pelvis (Fig 1). It is designed to keep the pelvic organs (bladder, uterus and rectum) in place and support spinal and pelvic stability. The pelvic muscles, which can be tightened at will, consist of two layers: a deep layer and a superficial one.

Source: Peter Lamb
The deep pelvic floor comprises the:
- Pubovisceral muscles, subdivided into the pubovaginalis, puborectalis and puboanalis muscles (these are sometimes called pubococcygeus muscles, although that term is more appropriately used when describing four-legged animals, on whom these muscles help with tail-wagging) (Peschers and DeLancey, 2008);
- Iliococcygeus muscle, a sheet of muscle that spans the pelvis from one side to the other;
- Puborectalis muscle, which maintains the anorectal angle, thereby, helping to prevent the leakage of faeces. Some of its fibres, along with the pubovisceral muscles, encircle the vagina to form the vaginal sphincter, which helps narrow the vaginal entrance Ashton-Miller and DeLancey, 2007; Dorey, 2003).
Each of the muscles has a different role within the pelvic floor: for example, the pubovaginal muscle elevates the anterior vaginal wall and urethra; damage to this could result in prolapse or/and urinary incontinence. Understanding the role of each muscle is vital for the prevention and treatment of stress urinary incontinence.
Together, the pubovisceral muscles and the iliococcygeus muscle form the levator ani muscles of the pelvic floor. The levator ani is what is most commonly known as ‘the pelvic floor muscles’; it is the target of pelvic floor exercises (see part 2).
The levator ani is composed of striated muscle fibres: two-thirds are slow-twitch fibres (type 1) while a third are fast-twitch fibres (type 2). Slow-twitch fibres maintain muscle tone at rest. Highly resistant to fatigue because they can contract over a long period of time, they give muscles endurance. Fast-twitch fibres exert 20% more force than slow-twitch fibres (Marques et al, 2010) and act quickly to reinforce their action Peschers and DeLancey, 2008). They tire quickly but can produce a strong and effective contraction; they also cope well with increases in intra-abdominal pressure.
Tightening the levator ani muscles enhances the effectiveness of the sphincter muscles, thereby, helping to prevent leakage and incontinence. This is especially the case when intra-abdominal pressure is raised, for example, on exertion, sneezing, coughing, laughing, lifting and straining.
The superficial muscles are made up of the bulbocavernosus and ischiocavernosus sphincter. The main function of the superficial pelvic floor muscles is to support and anchor the deep muscles to the pelvic girdle, but they also are active during sexual activity (Dorey, 2003).
The superficial pelvic floor muscles and sphincter muscles are innervated by the pudendal nerve, while the levator ani is innervated directly by the pelvic nerves. Any deficit in these nerves can be identified on examination of the dermatomes (Fig 2).

Source: Peter Lamb
Pelvic floor functions
Support and stability
The pelvic floor muscles support the female pelvic organs (bladder, uterus and rectum), protecting them against the effects of gravity. These muscles are an integral part of a wider muscle system that responds to increases in intra-abdominal pressure. They are also a key component of the ‘core’ muscles, which help the hips and spine to move, provide spinal and pelvic stability, and help maintain posture.
Continence
The muscles of the pelvic floor control the opening of the bladder and rectum, and maintain sphincter pressure and colorectal angle. They respond to an increase in intra-abdominal pressure (caused, for example, by coughing, sneezing, laughing or straining), which will cause them to contract around the urethra and anus to prevent leakage. They can also have an inhibitory effect on bladder activity. Just as importantly, they relax and lengthen to allow the passing of urine or faeces without straining.
Sexual function
In women, the voluntary contraction (squeezing) of the pelvic floor muscles contributes to sexual arousal and sensation. Sufficient strength of the pelvic floor muscles is necessary for orgasm, but excessive tension or sensitivity of the pelvic floor can contribute to pain during and/or after intercourse.
Pregnancy and childbirth
The pelvic floor muscles support the unborn child in the uterus during pregnancy, and help it navigate through the pelvic girdle during birth.
Causes of pelvic floor weakness
There are several factors that increase the risk of, or directly cause, damage to the pelvic floor muscles, leading to pelvic floor weakness or dysfunction. As explained by Marques et al (2010), many are a consequence of human evolution, childbirth and ageing. Others are lifestyle factors or illnesses. Causes of, and risk factors for, pelvic floor weakness are summarised in Box 1; the most prevalent causes and risk factors are also discussed below.
Pregnancy and childbirth
Pregnancy and childbirth are probably the biggest risk factors for pelvic floor damage. This is because, during pregnancy and childbirth, muscular, connective and nervous pelvic floor tissues are subjected to numerous anatomical, functional and hormonal modifications (Abrams et al, 2017). The pelvic floor goes through extensive change: initial hormonal changes prepare it for birth and it is stretched during vaginal delivery.
There are specific factors linked to pregnancy and childbirth that further increase the risk of damage to the pelvic floor:
- Baby’s weight of >4kg;
- Baby’s head circumference of >35.5cm;
- Mother’s age – mothers who are very young or middle-aged at first or last birth;
- Prolonged second stage of labour of >110mins;
- Vaginal delivery (versus Caesarean section).
The risk of pelvic floor damage is estimated to be 2.9 times higher after vaginal delivery than after Caesarean section (Abrams et al, 2017). During vaginal delivery, interventions such as episiotomy or use of forceps may be used and can cause tears (Abrams et al, 2017). These may, in turn, damage both internal and external anal sphincters, thereby, increasing the risk of faecal incontinence.
Chronic constipation
Constipation is the infrequent passage of hard stools and/or excessive straining when trying to defaecate. Chronic constipation and regularly having to strain to empty the bowels can overstretch and weaken the pelvic floor muscles. Difficulties emptying the bowels can sometimes be due to poor relaxation of the pelvic floor muscles.
Factors raising intra-abdominal pressure
Anything that continuously or repeatedly raises abdominal pressure puts extra strain on the pelvic floor and, therefore, risks damaging it (Spiteri and Kullar, 2008). Coughing, lifting, exercise and overweight have been reported to be risk factors for incontinence, as have, in particular, a body mass index of >30, high-impact exercise, and continual coughing due to smoking and/or a condition such as asthma. Heavy-weight and very vigorous gym activities with jumping can overload the pelvic floor muscles – this is particularly a risk in young healthy women.
Ageing and menopause
Pelvic floor dysfunction and incontinence become more common with age due to numerous age-related changes to body systems and organs. For example, the muscles of the bladder lose tone and elasticity, therefore, becoming less effective in controlling urine flow.
In women, the effects of ageing are compounded by the effects of the menopause. Throughout a woman’s lifespan, oestrogen levels fluctuate and this affects the amount of collagen fibres in pelvic floor muscles. This is particularly the case around the menopause, when oestrogen levels decrease and collagen fibres in pelvic floor muscles are depleted. The loss of collagen lowers the resistance and elasticity of pelvic floor muscles, making the pelvic floor thinner, drier and sometimes irritated and painful, which can lead to it becoming uncomfortable. This is also one reason why pelvic organ prolapse is more common in older women than in their younger counterparts – the thinner, weaker pelvic floor allows the bladder/bowel/vagina to descend into the pelvic area.
Box 1. Pelvic floor weakness: causes and risk factors
- Pregnancy and childbirth
- Chronic constipation
- Factors raising intra-abdominal pressure, including:
- Chronic coughing due to smoking and/or illness
- Heavy and/or repeated lifting
- High-impact exercise
- Being overweight or obese
- Ageing and menopause
- Surgery (such as hysterectomy, abdominal surgery) – this can cause trauma to the pelvic floor and a decrease in oestrogen levels
- Sexual abuse – this can cause trauma to the pelvic floor
- Neurological illness and especially connective tissue conditions, such as multiple sclerosis, rheumatoid arthritis, scleroderma – these can weaken the pelvic floor muscles
- Ethnicity – Hispanic and Caucasian women are at greater risk of pelvic floor weakness and dysfunction, as well as pelvic organ prolapse, than African and Asian women
Source: Abrams et al (2017)
Symptoms of pelvic floor weakness
A weakened pelvic floor can manifest symptomatically as urinary/faecal incontinence or pelvic organ prolapse. Both have their roots in the causes and risk factors described earlier. Continence problems due to pelvic floor weakness can affect both the bladder and bowel; the most common issues are outlined in Table 1.

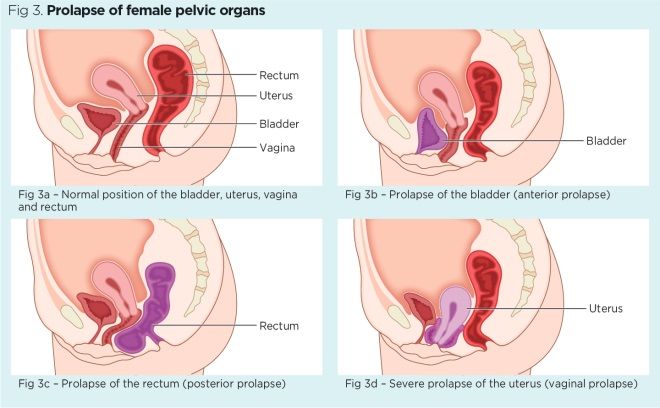
Pelvic organ prolapse (Fig 3) occurs when pelvic organs protrude into or out of the vagina. Anterior prolapse is caused by prolapse of the bladder (Fig 3b), posterior prolapse is caused by prolapse of the rectum (Fig 3c) and vaginal prolapse occurs when either the vagina or the uterus prolapse (Fig 3d). Prolapse is often described as heaviness, a ‘dragging’ feeling or ‘something coming down’; symptoms also include pain and/or discomfort in the vagina or abdomen and a lack of sensation during sexual intercourse.
Source: Peter Lamb
Conclusion
Pelvic floor weakness in women most often results from the accumulated exposure to risk factors such as pregnancy, childbirth and menopause over the lifetime. Women usually have a poor understanding of the anatomy and function of their pelvic floor muscles but they can protect their pelvic floor, or rehabilitate it if it has been weakened, with specific exercises. Part 2 of this two-part series (which comes with a journal club handout) discusses how to assess women’s pelvic floor health and teach them pelvic floor exercises.
Key points
- The pelvic floor is a complex group of muscles present in men and women
- A key function of the pelvic floor is to support urinary and faecal continence
- Women often lack knowledge about pelvic floor anatomy and function
- Pelvic floor weakness can lead to incontinence and pelvic organ prolapse
- Risk factors include high-impact exercise, obesity, pregnancy and childbirth, constipation and the menopause
Ashton-Miller JA, DeLancey JOL (2008) Functional anatomy of the female pelvic floor. In: Haslam J, Laycock J (eds) Therapeutic Management of Incontinence and Pelvic Pain – Pelvic Organ Disorders. London: Springer-Verlag London.
De Andrade RL et al (2018) An education program about pelvic floor muscles improved women’s knowledge but not pelvic floor muscle function, urinary incontinence or sexual function: a randomised trial. Journal of Physiotherapy; 64: 2, 91-96.
Dorey G (2003) Clench it or Drench It! A Self-help Guide for Ladies who Lunch, Laugh and Leak. Barnstaple: Grace Dorey.
Dumoulin C et al (2018) Pelvic floor muscle training versus no treatment, or inactive control treatments, for urinary incontinence in women. Cochrane Database of Systematic Reviews; 10: CD005654.
Marques A et al (2010) The status of the pelvic floor muscle training for women. Canadian Urological Association Journal; 4: 6, 419-424.
NHS England (2018) Excellence in Continence Care: Practical Guidance for Commissioners, and Leaders in Health and Social Care.
NHS England (2015) Excellence in Continence Care: Practical Guidance for Commissioners, Providers, Health and Social Care Staff and Information for the Public.
Peschers UM, DeLancey JOL (2007) Anatomy. In: Bo K et al (eds) Evidence-based Physical Therapy for the Pelvic Floor: Bridging Science and Clinical Practice. Philadelphia: Elsevier.
Yates A (2017) Incontinence and associated complications: is it avoidable? Nurse Prescribing; 15: 6.
 Nursing Times Resources for the nursing profession
Nursing Times Resources for the nursing profession

Have your say
or a new account to join the discussion.